What are SOAP Notes?
In healthcare settings, SOAP notes are a widely used method of documentation that allows healthcare professionals to record patient information in a structured and organized format. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, which are the four key components of a SOAP note.
These notes serve as a comprehensive record of a patient encounter, providing essential information for the care team.
Why Use SOAP Notes?
The use of SOAP notes offers several advantages in healthcare practice:
Enhanced Communication
One of the primary reasons to use SOAP notes is to improve communication among healthcare professionals. By following a standardized format with clear sections for subjective, objective, assessment, and plan, healthcare providers can convey essential information about the patient’s condition in a structured and organized manner. This facilitates the sharing of patient data, promotes collaboration among team members, and ensures that everyone involved in the patient’s care is informed and on the same page.
Improved Continuity of Care
SOAP notes contribute to improved continuity of care by creating a comprehensive record of each patient encounter. When healthcare providers document all relevant information in a structured format, it becomes easier to track the patient’s progress over time, monitor changes in their health status, and make informed decisions about their ongoing care. This continuity of information is particularly valuable in multidisciplinary care settings where multiple providers may be involved in the patient’s treatment.
Support for Legal and Professional Requirements
Proper documentation is essential to meeting legal and professional standards in healthcare practice. SOAP notes help healthcare providers fulfill these requirements by ensuring that all relevant information is recorded accurately, legibly, and in a timely manner. In cases where patient records are reviewed for legal or regulatory purposes, having well-documented SOAP notes can demonstrate the provider’s adherence to best practices and guidelines, reducing the risk of legal liability and supporting a high standard of care.
Facilitation of Clinical Reasoning
SOAP notes provide a structured framework for clinical reasoning, allowing healthcare providers to organize and analyze patient data systematically. By breaking down the encounter into subjective, objective, assessment, and plan sections, providers can methodically evaluate the patient’s symptoms, physical findings, diagnostic results, and treatment options. This structured approach promotes critical thinking, helps providers identify patterns or trends in the patient’s health status, and guides them in making evidence-based decisions about the most appropriate course of action for the patient’s care.
Overall, the use of SOAP notes in healthcare practice offers numerous benefits that contribute to the quality of patient care, support effective communication and collaboration among healthcare professionals, ensure compliance with legal and professional standards, and facilitate clinical reasoning and decision-making in the management of patient health.
What to Include in SOAP Notes?
When documenting patient encounters using SOAP notes, healthcare professionals should include specific information in each section to ensure a comprehensive and accurate record of the patient’s visit. Here are some guidelines on what to include in each component of a SOAP note:
Subjective
The subjective section of a SOAP note should capture the patient’s self-reported symptoms and medical history. It is essential to document the patient’s chief complaint, including the duration, severity, and associated symptoms of their condition. Additionally, healthcare providers should record the patient’s past medical history, current medications, allergies, social history, family history, and any other subjective information provided by the patient during the encounter.
Objective
In the objective section of a SOAP note, healthcare providers document measurable data obtained through physical examinations, diagnostic tests, and observations. This includes vital signs such as blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation. Providers should also record findings from the physical exam, including the appearance of the patient, palpation, auscultation, percussion, range of motion, and any other relevant assessments. In addition, any diagnostic tests, laboratory results, imaging studies, or other objective data should be included in this section.
Assessment
The assessment component of a SOAP note involves the healthcare provider’s clinical judgment regarding the patient’s condition. Based on the subjective and objective information gathered, the provider formulates a diagnosis or differential diagnosis, evaluates the patient’s progress, and determines the next steps in the management of the patient’s care. The assessment should be concise, relevant to the patient’s presenting problem, supported by the data collected, and clearly communicated to other members of the care team.
Plan
In the plan section of a SOAP note, healthcare providers outline the proposed course of action for the patient. This includes specific treatment options, medications prescribed, therapies recommended, referrals to specialists or other healthcare providers, diagnostic tests ordered, follow-up appointments scheduled, patient education provided, and any other interventions or actions planned to address the patient’s health needs. The plan should be tailored to the patient’s individual circumstances, preferences, and goals, and should be communicated clearly to the patient and other members of the care team.
By including these key components in each SOAP note, healthcare professionals can ensure that all pertinent information is documented in a clear and organized manner, supporting continuity of care, effective communication among the care team, and informed decision-making in the management of patient health.
How to Write Effective SOAP Notes
Writing effective SOAP notes requires attention to detail, clinical expertise, and strong communication skills. Here are some tips for healthcare professionals to consider when documenting patient encounters using SOAP notes:
1. Be Clear and Concise
When writing SOAP notes, it is important to be clear and concise in your documentation. Avoid using jargon or overly technical language that may be difficult for others to understand. Focus on conveying essential information in a straightforward manner that is easy to follow and interpret by other members of the care team.
2. Use Standardized Terminology
Using standardized medical terminology and abbreviations in SOAP notes helps ensure consistency and accuracy in documentation. Healthcare professionals should adhere to established guidelines and best practices for terminology to avoid confusion and misinterpretation of the information recorded in the notes.
3. Include Relevant Details
Include all relevant details in each section of the SOAP note to provide a comprehensive overview of the patient’s visit. Ensure that subjective information is specific and detailed, objective data is measurable and accurate, assessments are supported by evidence, and plans are tailored to the patient’s needs and preferences.
4. Document in Real-Time
Whenever possible, document patient encounters in real-time to ensure accuracy and completeness of the information recorded. Avoid relying on memory or delayed documentation, as this can lead to errors or omissions in the documentation that may impact patient care and decision-making.
5. Review and Revise as Needed
Review your SOAP notes regularly to ensure that they are up-to-date, accurate, and reflective of the patient’s current health status. Revise the notes as needed based on new information, changes in the patient’s condition, or updates to the care plan to maintain an accurate and relevant record of the patient’s care.
Tips for Writing Comprehensive SOAP Notes
Writing comprehensive SOAP notes requires attention to detail, critical thinking, and effective communication. Here are some additional tips for healthcare professionals to consider when documenting patient encounters using SOAP notes:
1. Be Thorough in Your Assessment
Conduct a comprehensive assessment of the patient’s condition, considering all aspects of their health and well-being. Document relevant physical findings, diagnostic test results, and observations to support your assessment and diagnosis. Include a detailed description of the patient’s symptoms, their duration, severity, and any factors that exacerbate or alleviate them.
2. Provide Rationale for Your Diagnosis
When formulating a diagnosis or differential diagnosis, provide a rationale for your clinical judgment based on the information gathered in the subjective and objective sections. Explain your reasoning, consider alternative diagnoses, and support your conclusions with evidence from the patient’s history, physical exam, and test results. Be transparent about the uncertainty or complexity of the diagnosis, if applicable.
3. Develop a Comprehensive Care Plan
Create a comprehensive care plan that addresses the patient’s needs holistically, taking into account their physical, emotional, and social well-being. Tailor the plan to the patient’s specific health goals, preferences, and circumstances. Include details on treatment options, medications, referrals, follow-up care, patient education, and self-management strategies to empower the patient in their health journey.
4. Monitor and Evaluate Patient Progress
Regularly monitor and evaluate the patient’s progress towards their health goals, reassessing their condition, and updating the care plan as needed. Document any changes in the patient’s status, response to treatment, or new developments that may impact their care. Use objective measures to track outcomes, assess the effectiveness of interventions, and adjust the plan accordingly to optimize patient outcomes.
5. Communicate Effectively with Patients
Engage patients in the documentation process by explaining the purpose of the SOAP notes, reviewing key findings, and discussing the proposed care plan with them. Use language that is easy to understand, free of medical jargon, and tailored to the patient’s level of health literacy. Encourage patients to ask questions, provide feedback, and actively participate in decisions about their care to promote shared decision-making and patient engagement.
By following these tips and best practices, healthcare professionals can write comprehensive SOAP notes that support high-quality patient care, effective communication, and informed decision-making in healthcare practice.
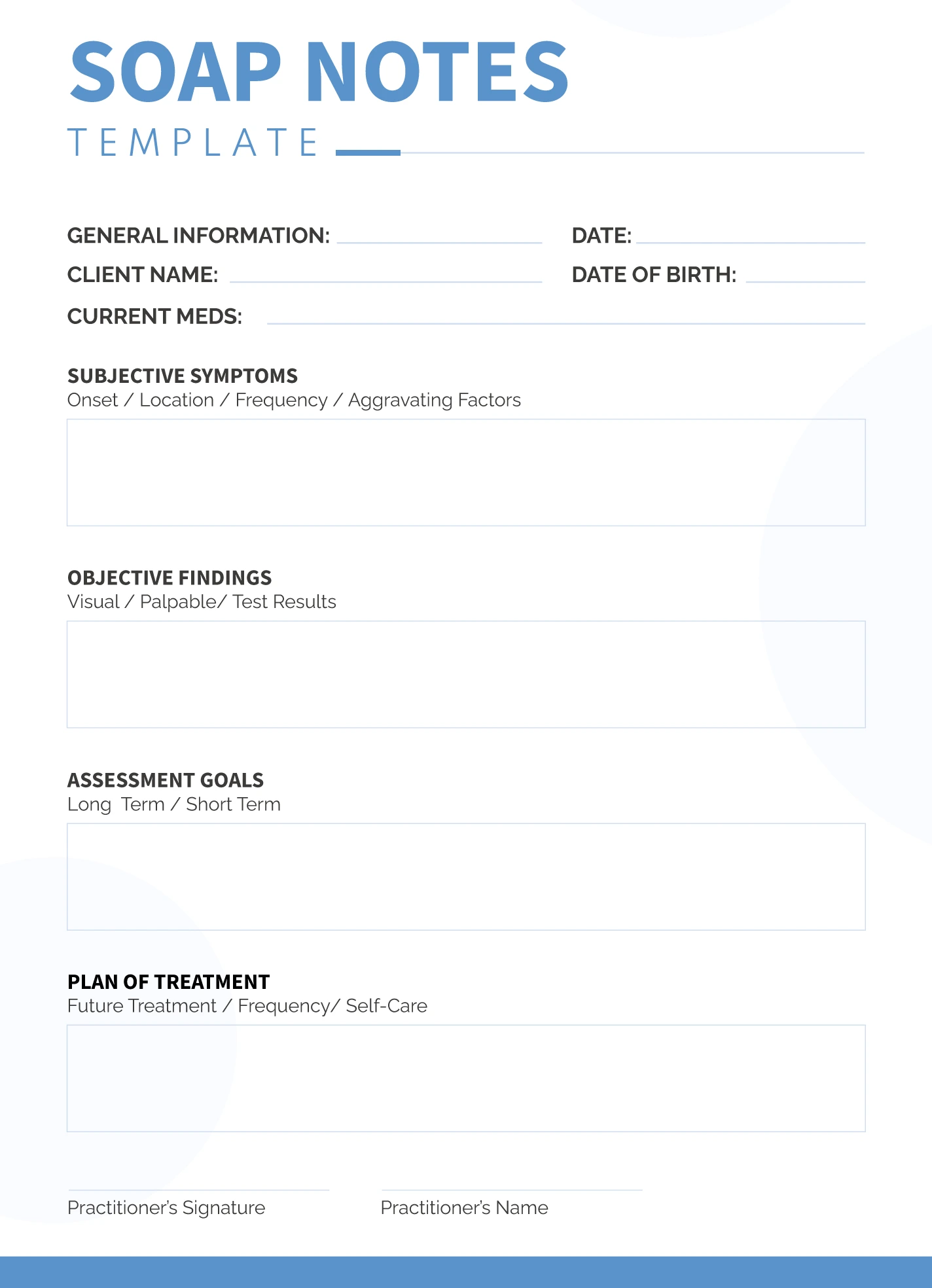
Free SOAP Note Template
In conclusion, a SOAP Note helps healthcare professionals document patient information in a clear, organized, and standardized format.
Improve communication and maintain accurate medical records—download our SOAP Note Template today to streamline your clinical documentation process!
SOAP Note Template – WORD